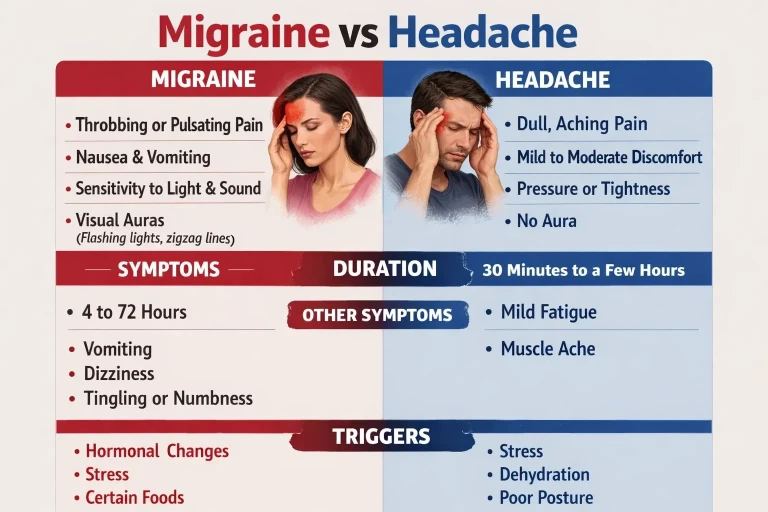
Migraines cause throbbing pain (usually one-sided) with nausea, light sensitivity, and can last 4-72 hours. Tension headaches feel like a tight band around your head with dull, pressing pain on both sides, without nausea or light sensitivity. While tension headaches affect up to 78% of Americans, migraines impact about 15% and are far more disabling.
Both headache types often originate from neck problems, which is why upper cervical chiropractic care can provide lasting relief for many sufferers.
Medical Disclaimer: This content is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before making any healthcare decisions or for guidance about specific medical conditions.
Understanding the Difference Matters
Knowing whether you have migraines or tension headaches isn't just an academic exercise—it directly affects which treatments will work for you. Many people mistakenly assume all headaches are the same, leading them to use ineffective treatments or miss opportunities for relief.
Research shows that 32% of patients initially diagnosed with tension headaches are later found to have migraines after more thorough evaluation. This misdiagnosis delays appropriate treatment and prolongs suffering. Understanding the distinct characteristics of each headache type helps you communicate more effectively with your healthcare provider and find solutions that actually work.
Migraine: More Than Just a Bad Headache
A migraine is a complex neurological condition, not simply an intense headache. It involves changes in brain chemistry, blood flow, and nerve signaling that create a cascade of debilitating symptoms. About 15% of American adults experience migraines, with women affected three times more often than men.
Classic Migraine Symptoms
Throbbing or pulsating pain: Usually on one side of the head, though it can switch sides or affect both
Moderate to severe intensity: Often rated 7-10 on a 10-point pain scale
Nausea and vomiting: Present in a majority of migraine attacks
Photophobia: Extreme sensitivity to light, often requiring a dark room
Phonophobia: Sensitivity to sound; normal conversation may feel painful
Worsens with activity: Physical movement, even walking, intensifies the pain
Duration: 4 to 72 hours if untreated
The Four Phases of Migraine
Many people don't realize migraines occur in distinct phases. Understanding these phases can help you recognize an attack early and take action.
1. Prodrome (Warning Phase): Hours to days before the headache, you may notice subtle changes: mood shifts, food cravings, increased thirst, neck stiffness, frequent yawning, or fatigue. About 60% of migraine sufferers experience prodrome symptoms.
2. Aura (For Some): About 20% of migraine sufferers experience aura—usually visual disturbances like flashing lights, zigzag lines, blind spots, or shimmering waves. Aura typically develops over 5-20 minutes and lasts less than an hour. Some people experience sensory or speech disturbances instead of visual symptoms.
3. Headache Phase: The main attack, with throbbing pain, nausea, and sensory sensitivities. This phase is what most people think of as "the migraine" and can last from 4 to 72 hours.
4. Postdrome ("Migraine Hangover"): After the headache resolves, many people feel drained, confused, or washed out for up to 24-48 hours. Some describe feeling euphoric or unusually refreshed, but fatigue is more common.
Common Migraine Triggers
- Hormonal changes (menstrual cycles, pregnancy, menopause)
- Stress and emotional tension
- Sleep disturbances (too much, too little, or irregular patterns)
- Certain foods (aged cheese, alcohol, processed meats, MSG)
- Caffeine (both excess intake and withdrawal)
- Weather changes and barometric pressure shifts
- Bright or flickering lights
- Strong odors
- Neck pain and cervical spine issues
Tension Headache: The Most Common Type
Tension headaches are the most common headache type, affecting up to 78% of Americans at some point in their lives. While generally less severe than migraines, they can significantly impact quality of life, especially when they become chronic.
Classic Tension Headache Symptoms
- Dull, aching pain: Often described as a "tight band" or "vise" around the head
- Bilateral location: Affects both sides of the head equally
- Mild to moderate intensity: Typically rated 3-6 on a 10-point pain scale
- Forehead, temple, or back of head: Pain may concentrate in these areas
- No nausea or vomiting: Unlike migraines, gastrointestinal symptoms are absent
- No light or sound sensitivity: You can usually function in normal environments
- Activity doesn't worsen pain: You can typically continue daily activities
- Neck and shoulder tightness: Muscle tension often accompanies the headache
Episodic vs. Chronic Tension Headaches
Episodic tension headaches occur fewer than 15 days per month. They may last 30 minutes to several days but have little impact on daily function. Most people experience this type occasionally.
Chronic tension headaches occur 15 or more days per month for at least 3 months. This type significantly affects quality of life and often requires professional treatment to manage effectively.
Common Tension Headache Triggers
- Stress and anxiety
- Poor posture (especially forward head position)
- Prolonged computer or phone use
- Muscle tension in neck, shoulders, and jaw
- Eye strain
- Fatigue and lack of sleep
- Dehydration
- Skipping meals
- Jaw clenching or teeth grinding
SEEK IMMEDIATE MEDICAL ATTENTION IF:
- Sudden, severe headache ("thunderclap") that peaks within seconds
- Headache with fever, stiff neck, confusion, or rash
- Headache after head injury
- Headache with vision loss, slurred speech, or weakness
- "Worst headache of your life"
- New headache pattern after age 50
These symptoms may indicate stroke, meningitis, aneurysm, or other serious conditions requiring emergency care.
The Neck Connection: Why Your Headaches May Start in Your Spine
Here's something that surprises many headache sufferers: over 75% of migraine patients report associated neck pain, and the vast majority of tension headaches are linked to muscle tension and postural issues originating in the neck. This isn't coincidental, it reflects the intimate connection between your cervical spine and headache generation.
The upper cervical spine (C1-C2) is located at the base of your skull, directly adjacent to the trigeminocervical complex, a network where the brainstem, upper spinal nerves, and the trigeminal nerve (responsible for facial and head sensation) converge. When the upper cervical vertebrae are misaligned, they can irritate this complex and trigger headache pain.
This explains why:
- Many headaches begin or worsen with neck stiffness
- Neck pain often precedes migraine attacks
- Poor posture correlates with increased headache frequency
- Correcting spinal alignment can reduce or eliminate headaches
- Treatment Approaches Compared
While medications can provide relief, they come with limitations:
- Medication Overuse Headaches: Taking pain relievers more than 2-3 times weekly can cause rebound headaches
- Side Effects: Many headache medications cause drowsiness, digestive issues, or other problems
- Symptom Management Only: Most medications treat symptoms without addressing underlying causes
- Variable Effectiveness: Up to 50% of migraine patients seek alternative therapies because medications don't work well enough
How Upper Cervical Chiropractic Care Addresses Both Headache Types
Evidence-based guidelines recommend spinal manipulation for both migraine and cervicogenic headaches. Upper cervical chiropractic care specifically targets the relationship between your neck and headache generation, addressing a root cause that medications cannot touch.
The Research
Clinical practice guidelines state that chiropractic care, including spinal manipulation, improves migraine and cervicogenic headaches
Studies show spinal manipulation may be as effective as some preventive medications for migraine, with fewer side effects
Over 80% of patients in one study reported stress as a major migraine factor, chiropractic care reduces the physical effects of stress on the neck
Low-load craniocervical mobilization has shown benefit for tension-type headache management
The Blair Approach
The Blair technique is specifically designed for the delicate upper cervical region:
- Precision Analysis: 3D imaging identifies your exact misalignment pattern
- Gentle Correction: No twisting or cracking, just a precise, light adjustment
- Lasting Results: Corrections often hold for weeks or months, reducing headache frequency
- Root Cause Focus: Addresses the spinal issues contributing to headache generation
By restoring proper alignment to the upper cervical spine, Blair chiropractic care can reduce irritation to the trigeminocervical complex, improve blood flow and nerve function, and decrease the muscle tension that triggers headaches.
Self-Help Strategies for Both Headache Types
While professional care often provides the most significant relief, these strategies can help reduce headache frequency and severity:
- Keep a Headache Diary: Track timing, duration, symptoms, and potential triggers to identify patterns
- Maintain Good Posture: Keep ears aligned over shoulders; avoid forward head position
- Take Regular Breaks: Every 30-60 minutes when working at a computer or desk
- Stay Hydrated: Dehydration is a common and preventable headache trigger
- Maintain Regular Sleep: Go to bed and wake at consistent times; aim for 7-8 hours
- Manage Stress: Practice relaxation techniques; regular exercise helps
- Limit Caffeine: Moderate intake and avoid sudden changes in consumption
Frequently Asked Questions
1. Can you have both migraines and tension headaches?
Yes—in fact, this is quite common. Some people experience distinct episodes of each type, while others develop "chronic migraine," where they have headaches on 15+ days per month with at least 8 having migraine features. The conditions can also trigger each other: tension and stress can precipitate migraines, and the muscle tension from migraine attacks can trigger subsequent tension headaches. This overlap is one reason why addressing cervical spine function can help both conditions.
2. Why do my headaches get worse with computer work?
Prolonged screen time creates a perfect storm for headaches. Forward head posture strains the upper cervical spine, eye strain triggers tension patterns, and sustained positions cause muscle fatigue. The resulting neck tension can trigger both tension headaches (through direct muscle pain) and migraines (through irritation of the trigeminocervical complex). Taking regular breaks, optimizing your workstation ergonomics, and addressing any underlying spinal issues can significantly reduce work-related headaches.
3. How quickly can chiropractic care help my headaches?
Response time varies based on headache type, chronicity, and individual factors. Some patients notice improvement within the first few visits, while others require several weeks of care before experiencing significant changes. In one case study, a patient with 40 years of chronic migraines experienced substantial improvement with upper cervical care. Generally, you should notice some change within 6-8 visits; if not, your provider should reassess the approach.
4. Are there any signs my headache needs emergency care?
Yes—certain headache characteristics require immediate medical evaluation: sudden severe headache reaching maximum intensity within seconds ("thunderclap"); headache with fever, stiff neck, rash, or confusion; new headache after age 50; headache after head trauma; or headache with neurological symptoms like vision loss, weakness, or difficulty speaking. These could indicate stroke, meningitis, aneurysm, or other serious conditions. When in doubt, seek emergency care.
5. Should I stop my medications if I try chiropractic care?
Never stop prescribed medications without consulting your prescribing physician. Chiropractic care can work alongside your current treatment plan. Many patients find they can gradually reduce medication use as their headaches improve, but this should always be done under medical supervision. Upper cervical care can be an effective complement to conventional treatment, not necessarily a replacement, at least initially.
6. Why haven't pain medications solved my headache problem?
Pain medications address symptoms, not causes. If your headaches originate from cervical spine dysfunction, muscle tension patterns, or postural issues, medications won't correct these underlying problems. Additionally, overusing pain relievers (more than 2-3 times weekly) can actually cause "medication overuse headaches," creating a cycle that's difficult to break. Addressing root causes through approaches like upper cervical care can provide more lasting relief.
Which Type of Headache Do You Have? Self-Assessment
Check all statements that describe your typical headache:
Section A: Migraine Indicators
- My headache pain is throbbing or pulsating
- Pain is usually on one side of my head
- I feel nauseous or sometimes vomit during headaches
- Light bothers me significantly during an attack
- Sounds are uncomfortably loud during headaches
- Physical activity makes my headache worse
- I sometimes see flashing lights or visual disturbances before headaches
- My headaches can last for days if untreated
Section B: Tension Headache Indicators
- My headache feels like pressure or tightness
- Pain affects both sides of my head equally
- I don't feel nauseous with my headaches
- Light and sound don't bother me much during headaches
- I can usually continue my activities despite the headache
- My neck and shoulders are often tight with headaches
- The pain is annoying but not severe
- Stress clearly triggers my headaches
Interpreting Your Results:
- Mostly Section A checked: Your headaches have migraine characteristics. Consider evaluation by a headache specialist or upper cervical chiropractor.
- Mostly Section B checked: Your headaches are consistent with tension-type headaches. Addressing posture, stress, and cervical spine function may help significantly.
- Mix of both sections: You may experience both types or have features that overlap. Professional evaluation can help clarify your headache pattern and guide treatment.
- Important: This self-assessment is informational only and cannot replace professional diagnosis. If you have frequent or severe headaches, consult a healthcare provider.
Ready for Professional Evaluation?
Contact Dennis Campbell, DC at our Wasco, California office to schedule your upper cervical assessment and discover if neck problems are contributing to your headaches.
What to Remember
- Migraines and tension headaches are different conditions with distinct symptoms, triggers, and treatment needs
- The neck-headache connection is significant: over 75% of migraine patients have associated neck pain
- Medications treat symptoms, not causes; addressing cervical spine issues can provide lasting relief
- Research supports spinal manipulation for migraine and cervicogenic headache management
- Blair upper cervical care uses gentle, precise adjustments to correct misalignments affecting headache patterns
References
Bryans R, et al. (2011). Evidence-based guidelines for the chiropractic treatment of adults with headache. Journal of Manipulative and Physiological Therapeutics, 34(5):274-89.
Chaibi A, Tuchin PJ, Russell MB. (2011). Manual therapies for migraine: a systematic review. Journal of Headache and Pain, 12(2):127-33.
Fernandez M, et al. (2023). Debate: differences and similarities between tension-type headache and migraine. Journal of Headache and Pain, 24(1):92.
GBD 2016 Headache Collaborators. (2018). Global, regional, and national burden of migraine and tension-type headache, 1990-2016. Lancet Neurology, 17(11):954-976.
International Headache Society. (2018). The International Classification of Headache Disorders, 3rd edition. Cephalalgia, 38(1):1-211.
Luedtke K, et al. (2016). Efficacy of interventions used by physiotherapists for patients with headache and migraine. Cephalalgia, 36(5):474-92.
Nelson CF, et al. (1998). The efficacy of spinal manipulation, amitriptyline and the combination of both therapies for the prophylaxis of migraine headache. Journal of Manipulative and Physiological Therapeutics, 21(8):511-9.
Tuchin PJ, et al. (2000). A randomized controlled trial of chiropractic spinal manipulative therapy for migraine. Journal of Manipulative and Physiological Therapeutics, 23(2):91-5.
Weber KT, et al. (2019). Integrating chiropractic care into the treatment of migraine headaches.
Global Advances in Health and Medicine, 8:2164956119835778.
WebMD. (2024). Tension Headache vs. Migraine: Differences, Symptoms, and Treatments. https://www.webmd.com/migraines-headaches/migraine-vs-tension-headache
_______________________________________________
Last medically reviewed: December 2025
Dennis Campbell, DC | Blair Upper Cervical Chiropractic | Wasco, California





Leave a comment