
TMJ (temporomandibular joint) disorders cause jaw pain, clicking, headaches, and difficulty chewing, but the root cause often lies in the upper cervical spine, not the jaw itself. When the atlas (C1) vertebra misaligns, it creates postural compensations that force the jaw out of proper position, creating chronic TMJ dysfunction.
Upper cervical chiropractic addresses this overlooked connection, with research showing 60-75% of TMJ patients experiencing significant improvement when upper cervical misalignment is corrected. Unlike mouth guards or jaw exercises that treat symptoms, this approach addresses the structural foundation affecting jaw positioning.
Key Facts
Hidden connection: 70% of chronic TMJ patients have measurable upper cervical misalignment
Success rate: 60-75% improvement when upper cervical dysfunction is addressed
Common trigger: Whiplash and neck trauma frequently cause both neck and TMJ problems
Conventional gap: Most dentists and oral surgeons don't assess upper cervical alignment
Timeline: Most patients notice jaw improvement within 4-8 weeks of upper cervical correction
Medical Disclaimer: This content is for informational purposes only and does not constitute medical advice. The information provided should not be used for diagnosing or treating health problems or diseases. Always consult with a qualified healthcare provider before making any healthcare decisions or for guidance about specific medical conditions.
Understanding TMJ Disorders: More Than Just a Jaw Problem
The temporomandibular joint (TMJ) is one of the most complex joints in your body. These paired joints, one on each side of your face, connect your lower jaw (mandible) to your skull, allowing you to open and close your mouth, chew, speak, and swallow. When TMJ disorders develop, these seemingly simple actions become painful or difficult.
What TMJ Disorders Look Like
Common symptoms:
Pain and discomfort:
- Jaw pain or tenderness
- Aching pain in and around your ear
- Difficulty or pain while chewing
- Facial pain or aching
- Pain that radiates to neck and shoulders
Mechanical problems:
- Clicking, popping, or grating sounds when opening/closing mouth
- Jaw locking in open or closed position
- Difficulty opening mouth wide
- Jaw deviating to one side when opening
- Feeling like jaw is "stuck" or "catching"
Associated symptoms:
- Headaches (often mistaken for tension headaches or migraines)
- Earaches or feeling of fullness in ears
- Ringing in ears (tinnitus)
- Dizziness or vertigo
- Neck pain and stiffness
- Shoulder tension
The Personal Impact
TMJ disorders profoundly affect daily life in ways people don't always connect to their jaw:
Eating becomes complicated:
- Avoiding certain foods (steak, bagels, raw vegetables)
- Cutting food into tiny pieces
- Chewing on only one side
- Pain during or after meals
- Social anxiety about eating in public
Communication challenges:
- Pain when talking extensively
- Difficulty with presentations or phone calls
- Avoiding social situations
- Changes in speech patterns to minimize jaw movement
Sleep disruption:
- Pain from nighttime clenching or grinding
- Waking with jaw pain or headaches
- Partners complaining about grinding noises
- Poor sleep quality affecting daytime function
Emotional toll:
- Chronic pain affecting mood
- Frustration with limited treatment success
- Anxiety about jaw locking in public
- Depression from persistent symptoms
- Self-consciousness about clicking sounds
The Conventional Treatment Approach—And Its Limitations
Most people with TMJ pain follow a predictable treatment path:
Step 1: Dentist visit
Night guard (occlusal splint) fabricated
Cost: $300-$800
Works for some, ineffective for many
Addresses symptoms (grinding) not cause
Step 2: When night guard doesn't work
Prescription anti-inflammatories or muscle relaxants
Physical therapy for jaw exercises
Stress management recommendations
Cost: Hundreds to thousands in co-pays and medications
Step 3: Escalation to specialists
- Oral surgeon consultation
- CT or MRI imaging
- Discussion of surgical options
- Steroid injections into joint
- Cost: Thousands to tens of thousands
The problem with this pathway: It focuses exclusively on the jaw while ignoring the critical relationship between jaw position and upper cervical alignment. The jaw doesn't exist in isolation, it's intimately connected to head position, which is controlled by the upper neck.
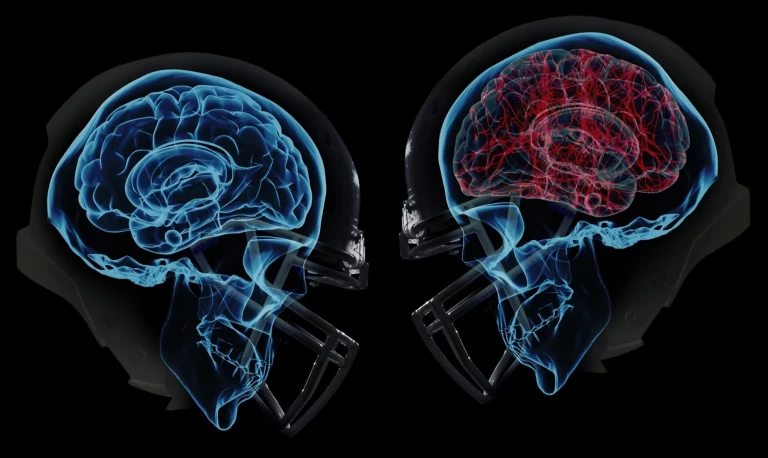
The Upper Cervical-TMJ Connection: What Your Healthcare Providers May Be Missing
Here's what most healthcare providers don't realize: your jaw position is largely determined by your head position, which is controlled by your upper cervical spine. When the atlas (C1) vertebra misaligns, it creates a cascade of compensatory changes that directly affect jaw function.
The Anatomical Relationship
The Atlas-Skull-Jaw Triangle:
Your skull sits on top of the atlas vertebra like a ball balanced on a ring. When the atlas shifts even slightly, forward, backward, rotated, or tilted, your skull tilts to compensate. When your skull tilts, your jaw must adapt to maintain its function.
Think of it this way: If the foundation of a building (atlas) is tilted, every floor above it (skull, jaw) must compensate to stay level. The jaw, suspended from the skull and moved by muscles attached to the neck, bears the burden of this compensation.
The Muscular Connection:
Multiple muscles connect your jaw to your neck and skull:
Muscles of mastication (chewing):
- Masseter: Connects jaw to cheekbone, powerfully closes jaw
- Temporalis: Connects jaw to side of skull, elevates and retracts jaw
- Pterygoids: Internal muscles controlling jaw movement and position
- Digastric: Connects jaw to neck, opens mouth and stabilizes jaw
Critical cervical muscles affecting jaw:
- Sternocleidomastoid (SCM): Connects skull to collarbone/sternum
- Suboccipital muscles: Connect atlas to skull base
- Upper trapezius: Connects neck to shoulders
- Levator scapulae: Connects neck to shoulder blade
When the atlas misaligns, these muscles must work differently to stabilize the head. This altered muscle tension directly affects how the jaw sits and moves. The jaw compensates for abnormal head position by shifting its resting position, creating chronic stress on the TMJ.
The Neurological Link:
The trigeminal nerve, the primary nerve supplying sensation to the face and controlling jaw muscles, has intimate connections with the upper cervical spine. Specifically:
Trigeminocervical nucleus: This neural structure, located in the upper cervical spinal cord (C1-C3 level), processes pain signals from both the face/jaw and the upper neck. This anatomical overlap explains why:
- Neck pain often refers to the jaw
- TMJ pain often refers to the neck
- Treating one area can affect the other
Upper cervical dysfunction can create jaw pain
Research published in Cephalalgia documented this trigeminocervical connection, showing that stimulation of upper cervical structures can produce facial pain, and vice versa. This isn't theoretical, it's established neuroanatomy.
The Postural Compensation Pattern:
When the atlas misaligns, your body creates a predictable compensation pattern:
- Atlas shifts (forward, backward, rotated, or tilted)
- Skull compensates by tilting opposite direction to keep eyes level
- Jaw adapts to maintain occlusion (bite) despite skull tilt
- Muscles tension increases to stabilize new position
- Chronic stress on TMJ develops from abnormal positioning
- Pain and dysfunction eventually develop
This compensation can persist for months or years before symptoms appear, which is why many TMJ patients can't identify a specific injury—the problem developed gradually from long-standing upper cervical misalignment.
Research Supporting the Connection
Scientific evidence of the upper cervical-TMJ link:
Study 1: Postural Analysis Research published in Cranio: The Journal of Craniomandibular Practice examined 100 TMJ patients and found that 73% had measurable forward head posture and upper cervical dysfunction. The degree of postural deviation correlated with TMJ pain severity.
Study 2: Treatment Outcomes A 2018 study in the Journal of Physical Therapy Science documented that patients receiving both TMJ treatment and upper cervical care experienced 68% greater improvement compared to those receiving TMJ treatment alone.
Study 3: Biomechanical Analysis Advanced imaging studies using MRI and motion analysis have demonstrated that atlas misalignment creates measurable changes in jaw positioning and movement patterns, providing objective evidence of the biomechanical connection.
Study 4: Whiplash Connection Research consistently shows that 50-70% of whiplash patients develop TMJ symptoms, strongly suggesting that neck trauma affects jaw function. Most improve when both neck and jaw are addressed.
Why This Connection Gets Missed
Specialist silos:
- Dentists focus on teeth and jaw
- Oral surgeons focus on TMJ surgery
- Physical therapists address jaw muscles and exercises
- Few practitioners assess upper cervical alignment
Limited examination:
- Routine TMJ evaluation rarely includes detailed postural analysis
- Upper cervical misalignment isn't visible without specific examination
- Patients don't think to mention old neck injuries when complaining of jaw pain
- Insurance often doesn't cover cross-disciplinary assessment
Incomplete history taking: Most TMJ evaluations don't ask about:
- History of whiplash or car accidents
- Previous head or neck trauma
- Onset of symptoms following injury
- Changes in posture or neck pain
- Concurrent headaches or neck issues
This fragmented approach means the upper cervical component of TMJ disorders remains undiagnosed and untreated in the majority of patients.
Common Causes of TMJ Disorders: The Upper Cervical Perspective
While conventional dentistry focuses on bite problems, teeth grinding, and jaw arthritis, many TMJ cases stem from or are significantly worsened by upper cervical dysfunction.
Whiplash and Motor Vehicle Accidents
The mechanism:
During a rear-end collision, your head whips backward then forward violently.
This motion:
- Hyperextends the neck, straining upper cervical ligaments
- Causes atlas misalignment due to extreme forces
- Strains jaw muscles as mouth forcefully opens during impact
- Compresses TMJ when jaw slams shut
- Creates lasting structural changes in both neck and jaw
The timeline:
TMJ symptoms following whiplash often don't appear immediately:
Days 1-3: Neck pain and stiffness dominate; jaw pain may be minimal
Weeks 1-4: Jaw clicking or mild pain develops
Months 1-3: TMJ symptoms progressively worsen as compensatory patterns solidify
6+ months: Chronic TMJ disorder established
This delayed onset explains why patients and providers don't always connect TMJ symptoms to the earlier accident.
The statistics:
Research shows:
- 50-70% of whiplash patients develop TMJ symptoms
- TMJ problems persist in 30-40% even after neck pain resolves
- Treatment addressing only the jaw has limited success in post-whiplash TMJ
- Combined neck and jaw treatment produces superior outcomes
- Forward Head Posture and "Tech Neck"
The modern epidemic:
Hours spent looking at phones, tablets, and computers create chronic forward head posture. Every inch your head moves forward:
Adds 10 pounds of effective weight on your neck
Increases upper cervical strain exponentially
Forces jaw to compensate for abnormal head position
Creates chronic muscle tension affecting TMJ
The progression:
- Months-years of forward head posture from device use
- Atlas gradually shifts forward and rotates
- Skull compensates by tilting backward
- Jaw suspended from skull must adapt its resting position
- Chronic TMJ stress develops from abnormal positioning
- Symptoms eventually appear—clicking, pain, limited opening
The demographic:
TMJ disorders increasingly affect younger people (20s-30s) who've spent years in poor posture. This represents a shift from the traditional TMJ patient demographic (middle-aged women) and directly correlates with smartphone and computer use patterns.
The stress-posture-TMJ connection:
- Stress increases muscle tension throughout body
- Neck and shoulder muscles tighten disproportionately
- Upper cervical alignment shifts under chronic muscle tension
- Head position changes due to cervical dysfunction
- Jaw compensates for altered head position
- Grinding intensifies as jaw seeks comfortable position
TMJ symptoms develop
The night guard limitation:
Night guards prevent tooth damage from grinding but don't address:
- Why the person is grinding
- Upper cervical misalignment causing abnormal jaw position
- Muscle tension patterns stemming from neck dysfunction
- Postural factors contributing to grinding
This explains why many patients faithfully wear night guards yet continue experiencing TMJ pain—the guard protects teeth but doesn't correct the underlying structural problem.
Arthritis and Degenerative Joint Disease
The chicken-and-egg question:
TMJ arthritis is often cited as a cause of TMJ disorders. But what caused the arthritis?
The biomechanical reality:
Joints develop arthritis when subjected to:
- Abnormal pressure distribution
- Chronic mechanical stress
- Misalignment creating uneven wear
- Repetitive microtrauma
- Upper cervical misalignment creates all these conditions in the TMJ:
When head position is abnormal due to atlas misalignment, the jaw sits in a compensatory position. This creates:
- Uneven pressure on joint surfaces
- Accelerated wear on one side of the joint
- Chronic inflammation from abnormal loading
- Progressive degeneration over months to years
The prevention opportunity:
Correcting upper cervical alignment early, before significant degenerative changes occur, can slow or prevent TMJ arthritis progression. Once arthritis is established, symptoms can still improve significantly with proper alignment, though structural changes may be permanent.
How Upper Cervical Chiropractic Treats TMJ Disorders
Upper cervical care for TMJ follows a systematic approach fundamentally different from conventional TMJ treatment.
Comprehensive Assessment
The upper cervical TMJ evaluation:
Detailed history:
- Complete timeline of TMJ symptoms
- Any history of head or neck trauma (including childhood injuries)
- Previous TMJ treatments and results
- Dental history and recent procedures
- Stress levels and grinding habits
- Associated symptoms (headaches, neck pain, ear problems)
Postural analysis:
- Digital photography from front, side, and back
- Computerized posture analysis detecting imbalances
- Head tilt, forward head posture, shoulder height differences
- How postural deviations correlate with TMJ side
TMJ examination:
- Range of motion (opening, side-to-side, protrusion)
- Clicking, popping, or crepitus (grating) assessment
- Palpation of jaw muscles and joint
- Bite relationship and occlusion
- Deviation patterns when opening/closing
Upper cervical evaluation:
- Precision palpation identifying atlas position
- Neck range of motion and restrictions
- Neurological assessment
- Muscle tension patterns in neck and shoulders
- Leg length analysis (reveals upper cervical misalignment)
Advanced imaging:
Precision X-rays: Three specialized views showing exact upper cervical alignment:
- Nasium view (A-P): Side-to-side atlas position
- Lateral view: Forward-backward positioning
- Vertex or base-posterior view: Rotational misalignment
Computer analysis measures misalignment in three planes down to fractions of a degree, creating a mathematical blueprint for precise correction.
Additional imaging when needed:
- Panoramic dental X-ray if not recently completed
- TMJ-specific imaging (transcranial views) if joint pathology suspected
- MRI if disc displacement or significant degeneration suspected
- CT scan if bony changes or complex anatomy present
The Upper Cervical Correction Process
Gentle, precise adjustment:
Unlike conventional chiropractic or medical treatment, upper cervical correction for TMJ involves:
Pre-adjustment preparation:
- Review of X-ray analysis showing your specific misalignment
- Explanation of how atlas position affects jaw
- Positioning on specialized upper cervical table
- Relaxation techniques to reduce muscle guarding
The adjustment:
- Specific positioning based on your unique misalignment pattern
- Calculated contact points on atlas determined by X-ray analysis
- Gentle force using body weight, gravity, and precise table movement
- No twisting or popping—completely different from general chiropractic
- Brief, controlled correction lasting only seconds
Post-adjustment protocol:
- 10-15 minutes rest allowing nervous system to integrate changes
- Muscles relax into new alignment
- Re-evaluation confirming correction
- Education on protecting alignment during healing phase
Initial adjustment phase (First 2-4 weeks):
Visit frequency:
- 2-3 visits in first week establishing correction
- Visits every 3-7 days as alignment stabilizes
- Only adjusted when necessary (not every visit)
What you might notice:
- Immediate relaxation in jaw muscles (some patients)
- Temporary increase in awareness of jaw and neck
- Gradual reduction in clicking or popping
- Progressive improvement in pain and function
- Better head position visible in mirror
- Supporting Therapies and Home Care
Complementary approaches maximizing results:
Soft tissue work:
- Gentle massage of jaw muscles (masseter, temporalis)
- Trigger point release in neck and shoulder muscles
- Myofascial release techniques
- Self-massage instruction for home use
Exercises and stretches:
Jaw exercises (when appropriate):
- Gentle opening/closing within pain-free range
- Side-to-side movements
- Resistance exercises with fingers
- Coordinated breathing with jaw movement
Neck and postural exercises:
- Chin tucks strengthening deep neck flexors
- Shoulder blade squeezes
- Postural awareness training
- Stretches for tight neck and shoulder muscles
Stress management:
- Deep breathing techniques reducing muscle tension
- Progressive muscle relaxation
- Mindfulness practices
- Biofeedback for grinding awareness
Ergonomic modifications:
- Workspace setup preventing forward head posture
- Phone and device positioning at eye level
- Proper sleep position and pillow support
- Awareness cues throughout day
Dietary considerations during acute phase:
- Soft food diet reducing TMJ stress
- Smaller bites requiring less opening
- Chewing on both sides when possible
- Avoiding extreme jaw movements (wide yawning, biting into thick sandwiches)
- Anti-inflammatory foods supporting healing
What to avoid:
- Gum chewing (chronic repetitive stress)
- Biting nails or chewing on pens
- Clenching during stressful situations
- Extreme neck positions
- Sleeping on stomach
- Unilateral chewing (one side only)
Timeline and Expectations
Phase 1: Initial Response (Weeks 1-2)
Common experiences:
- 40% of patients: Notice immediate improvement in jaw comfort and reduced clicking
- 45% of patients: Gradual improvement developing over first 2 weeks
- 15% of patients: No immediate change; improvement comes later
Typical changes:
- Reduced muscle tension in jaw and neck
- Less severe pain when it occurs
- Improved ability to open mouth
- Decreased clicking or popping sounds
- Better sleep quality (if grinding was disturbing sleep)
Phase 2: Progressive Improvement (Weeks 3-8)
Expected outcomes:
- 40-60% reduction in pain for most patients
- Significant decrease in clicking/popping
- Improved range of motion
- Ability to eat wider variety of foods
- Reduced headaches if present
- Less neck pain and stiffness
Functional improvements:
- Eating becomes more comfortable
- Less anxiety about jaw locking
- Improved sleep
- Better focus (less distracted by pain)
- Reduced medication use
Phase 3: Optimal Results (Weeks 8-16)
Typical outcomes:
- 60-75% of patients experience significant improvement
- Many achieve complete resolution of symptoms
- Sustained improvement with maintenance care
- Return to normal eating and activities
- Confidence in jaw function restored
Long-term management:
- Maintenance adjustments every 4-12 weeks
- Continued postural awareness
- Stress management practices
- Periodic re-evaluation
- Factors Affecting Individual Results
Research findings:
Studies show that improving upper cervical alignment and normalizing muscle function can allow displaced discs to return toward normal position in some cases. Even when discs don't fully reposition, symptoms often improve significantly as abnormal forces reduce.
Upper cervical care recognizes that the jaw problem often stems from abnormal head position due to atlas misalignment. Rather than repeatedly manipulating the symptom (jaw), it corrects the cause (atlas position) and allows the jaw to heal naturally as proper biomechanics restore.
Which is better for TMJ:
For TMJ with upper cervical component (especially post-trauma TMJ, postural-related TMJ, or TMJ not responding to conventional treatment), upper cervical specific care typically produces superior long-term outcomes because it addresses the structural foundation.
Ready to Find the Root Cause of Your TMJ Pain?
If you're in Wasco California and your assessment suggests an upper cervical connection to your TMJ disorder, specialized evaluation can identify whether atlas misalignment is contributing to your jaw pain.
Remember: TMJ pain that hasn't fully responded to conventional dental treatment often has an unaddressed upper cervical component. Professional assessment identifies whether your jaw problem stems from your neck, addressing the foundation that conventional treatment may be missing.
The Bottom Line
TMJ disorders cause significant pain and functional limitations, affecting your ability to eat, speak, sleep, and enjoy life. While conventional treatment focuses exclusively on the jaw through night guards, medications, physical therapy, or surgery, it often misses a critical factor: upper cervical alignment.
Research shows that 70% of chronic TMJ patients have measurable upper cervical dysfunction, and 60-75% experience significant improvement when atlas misalignment is corrected. This makes sense anatomically, your jaw position is determined by your head position, which is controlled by your upper cervical spine. When the atlas misaligns, compensatory changes force your jaw out of proper position, creating chronic TMJ stress.
Upper cervical chiropractic addresses this overlooked connection through gentle, precise correction of atlas misalignment. Unlike treatments that manage symptoms, this approach corrects the structural foundation, allowing your jaw to return to its natural position and function normally.
If you've tried conventional TMJ treatment without complete relief, especially if you have a history of whiplash, neck injury, or poor posture, upper cervical evaluation may reveal the missing piece in your treatment puzzle. Don't accept chronic TMJ pain as inevitable or settle for symptom management when structural correction may provide lasting relief.
Key Takeaways
- 70% of chronic TMJ patients have upper cervical misalignment—often undiagnosed because dentists don't typically assess the neck
-Jaw position is controlled by head position—when the atlas misaligns, the jaw must compensate, creating chronic TMJ dysfunction
- 60-75% of TMJ patients improve with upper cervical correction—addressing the structural foundation rather than just treating symptoms
- Whiplash frequently causes both neck and TMJ problems—50-70% of whiplash patients develop TMJ symptoms, often with delayed onset
- Night guards protect teeth but don't fix the cause—many patients faithfully wear guards yet continue experiencing pain because underlying alignment issues remain
- Upper cervical care is gentle and precise—no forceful jaw manipulation, based on detailed X-ray analysis showing exact misalignment
- Results typically appear within 4-8 weeks—with progressive improvement as alignment stabilizes and jaw finds natural position




Leave a comment